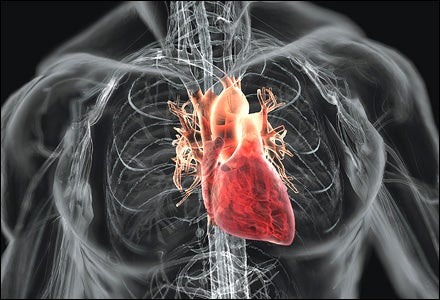
Put your hand on your chest or your finger on your carotid artery and find your heartbeat. Got it? Now give that rhythm your undivided attention. Your heart thumps some 100,000 times daily, but how often do you give this vital organ its due? Not often enough, according to the latest research. Despite proven prevention and treatment plans, heart disease remains the number-one killer in the U.S. More than one million Americans suffer heart attacks each year, with about half proving fatal. And while heart-attack rates go up sharply after age 45, men 29 to 44 years old┬Śsome of them seemingly healthy athletes┬Śstill account for about 34,000 cases annually. To help keep your risk low┬Śnow and for decades to come┬Śwe’ve gathered expert advice from cardiologists, trainers, and nutritionists on how to best protect this all-important muscle. You just might want to keep your hand where it is while you read on.
The Pump House
Pump House
 Bryan Christie
Bryan Christie
How It Works
The heart has four chambers that pump, on average, about 2,000 gallons of blood per day. The upper chambers are called the atria, and the lower chambers, the ventricles.
The left atrium (1) receives oxygenated blood from the lungs via the pulmonary vein.
The blood then passes through the mitral valve (2) into the left ventricle (3). The left ventricle is the largest and strongest chamber, with walls about half an inch thick.
When the left ventricle is full, it contracts. Simultaneously, the mitral valve snaps closed like a trapdoor (preventing backflow) and the aortic valve opens, allowing the blood to flow into the aorta (4)┬Śthe body’s largest blood vessel. It routes oxygen-rich blood through the body.
The right atrium (5) receives oxygen-depleted blood via two veins: the superior vena cava, from the upper body, and the inferior vena cava, from the lower body.
The tricuspid valve (6) opens to allow thedepleted blood to flow into the right ventricle (7).
As the right ventricle contracts, the tricuspid valve closes and the pulmonary valve opens, allowing blood to flow into the pulmonary artery and then to the lungs.
Meanwhile, the heart itself is a muscle that needs oxygen-rich blood, and this is delivered through coronary arteries that branch off of the aorta.
The heart’s left side is larger because it pumps blood to the entire body.
How It Fails
Big MI coming! That’s what doctors, at least the ones that play them on TV, like to say when a heart-attack patient comes wheeling into the ER. It stands for myocardial infarction, which means your heart’s blood supply is cut off, usually the result of coronary-artery disease. CAD is a hardening of the arteries due to atherosclerosis, a fancy way of saying there’s gunk in the plumbing┬Śthat is, your arteries are clogged with plaque, a by-product of cholesterol. In its milder form, CAD results in reduced blood flow to the heart and a feeling of tightness in the chest or outright pain (called angina). If an artery becomes completely blocked┬Śusually when a bit of plaque bursts and a blood clot forms┬Ślack of oxygen means heart tissue will start dying within half an hour.
Tune Up
Express Train
Forget your maximum heart rateAt Carmichael Training Systems, we’ve learned in the past few years that the best way to gauge your workouts is with your max sustainable heart rate. To find it, ride or run as fast as you can for 15 minutes, using a heart-rate monitor to capture your average heart rate over that period. Then, for hard interval rides, stay close to 92 to 95 percent of that number. (Or 96 to 98 percent for runs.) For endurance rides, keep a moderate pace┬Śdon’t let your pulse get above 88 percent. (Runners, stay below 95 percent.) On recovery sessions, stay below 70 percent to reap the greatest benefits (85 percent and lower for runners).
┬ŚChris Carmichael
Tune Up

Prescribing exercise for your heart is like buying wine for a dinner party. You know it’s a good idea, but what kind? How much? The good news: Even a small amount of aerobic activity yields some benefit. The better news: Optimum heart health requires a combination of intense cardio work and mellow endurance sessions┬Śwhich will pay off on race day as well. Here’s what the experts say:
Do Something┬ŚAnything!
Work, family, hammocks… All kinds of distractions can thwart your training plans, but don’t give up completely. Strive to get at least 30 minutes per day of moderate-intensity aerobic activity. All forms of cardio work do the trick: running, cycling, team sports, swimming, and treadmills and other stationary trainers. No time for a quick workout? Yard work and even riding your cruiser to the office count. A Harvard Alumni Health study found that heart-disease risk starts declining when you burn just 1,000 calories per week (about two hoursof running at a ten-minute-per-mile pace).
Step It Up
A rigorous training plan dovetails nicely with a smart heart regimen. Mix intervals into your workouts; they improve your performance at lactate threshold and help train your heart to work more effectively and recover more quickly. Do at least one or two interval sessions weekly, reaching your maximum sustainable heart rate (see “Express Train,” above) during three to four high-intensity efforts of up to ten minutes each (adjust for training goals). Slow to a recovery pace between intervals.
Perform endurance workouts at least three times per week. You should be able to maintain a conversation during these moderately paced efforts. Distance will vary. If you’re training for a competition, build mileage gradually until you’re covering at least 75 percent of your race-day mileage.
Test Your Ticker
Heart Health Q & A
An elite athlete seems to drop dead of heart failure every year. Why?First, cardiac arrest in fit young athletes is a rare phenomenon that guarantees media attention. Still, Dr. Steven Van Camp, a sports cardiologist at UC Irvine Medical Center, says, “If it prompts athletes to call their doctor and get a long-overdue health check, that’s not necessarily bad.” Likely culprits? Congenital problems or coronary-artery disease, which a thorough exam can reveal. “The person who gets into trouble is the person who has a condition and doesn’t know it or has a condition and doesn’t deal with it,”says Van Camp.
Test Your Ticker
Here are two easy ways to get a quick measure of heart health.
(1) Go to the National Institutes of Health’s online risk-assessment calculator () to learn your odds of having a heart attack within the next ten years.
(2) How quickly your heart recovers from exercise is also a good indicator. Give yourself this simple test, based on a study published in The New England Journal of Medicine.
╠ř
Step 1: Run for ten minutes at a moderate to vigorous pace (fast enough that it’s difficult to carry on a conversation). Immediately after stopping, check your heart rate (count beats per minute with a watch or use a heart-rate monitor).
Step 2: After the initial reading, wait one minute and calculate your heart rate again.
Step 3: Do the math. Your heart rate should have dropped by at least 25 beats per minute. If it didn’t, you should see a cardiologist and make some lifestyle changes. In the NEJM study, participants whose heart rate dropped fewer than 25 beats per minute were more likely to suffer heart attacks.
╠ř
Lower Your Risk

Heart Health Q & A
When I overeat, can I do anything to make amends?So you lost all willpower and scarfed down a double cheeseburger with all the fixings, onion rings, and a shake? It’s not too late to make peace with your arteries. According to a 2006 study published in the European Journal of Applied Physiology, doing some sort of physicalactivity immediately following a fatty meal can reverse your dinner’s artery-clogging effects. You’ll likely be in no condition for anything more rigorous than a brisk walk, but fortunately that should do the trick.
Of all the idiot ways to bite the dust, heart disease ranks right up there with BASE jumping into a strong headwind. In both cases, poor choices are almost always to blame. A 2004 study called Interheart found that 90 percent of first heart attacks in men (and 94 percent in women) can be attributed to risk factors that are largely in your control. Here are the key factors cited by Interheart, the American Heart Association, and the CDC.
1. Cigarette smoking. You know this. But did you know that smoking just once a month increases risk of heart disease? Cigarette smoking raises your blood pressure and clogs your arteries. Among men aged 35┬ľ39, smokers are five times more likely to have a heart attack than nonsmokers. And Bill Clinton notwithstanding, you don’t get a free pass for not inhaling. Even cigars raise therisk of death from heart disease, though not as significantly as cigarettes.
Solution: Quit. Even on poker night.
2. High cholesterol. You need to know three things about cholesterol: LDL (“bad”) cholesterol causes arterial plaque, the fatty deposits that clog or block blood flow; HDL (“good”) cholesterol helps clear arteries; and all adults should have their cholesterol levels checked every three to five years, starting in their twenties. The key numbers: Keep your LDL cholesterol count under 100 mg/dl, your HDL above 40, and the total under 200.
Solution: Maintain healthy cholesterol levels through regular exercise and a smart diet (see “Eat Like a Greek,” below). If necessary, statin drugs have proven effective at lowering cholesterol, as have high doses of niacin (vitamin B3).
3. High blood pressure. Like cholesterol levels, your blood pressure can be dangerously high without any outward warning signs. Nearly one in three adults have high blood pressure, but as many as 30 percent of them don’t know it. Left unchecked in your twenties and thirties, both problems can lead to clogged arteries later. Your blood pressure should be under 120/80; have it checked at least once a year.
Solution: Consume less salt, exercise, and relax.
4. Diabetes. It’s been called an epidemic, and it’s hard to argue with 20 million cases of diabetes nationwide.
Solution: Keep your weight in control. Done that? Decrease sugar intake, and lose 5 to 7 percent of your body fat.
5. Obesity. A spare tire around your waist often means fat around your heart.
Solution: Lose the gut. And remember: It’s possible to be thin and still have internal fat deposits due to poor diet.
6. Stress. It elevates blood pressure, which increases heart-attack risk. A study published in the May 22 issue of the Journal of the American College of Cardiology concluded that subjects with the highest levels of anxiety had twice the heart-attack risk of those with the lowest.
Solution: Relax, take up yoga, and avoid stressful situations. Yes, you now have a medical excuse to skip that weekend with the in-laws.
7. Poor diet. Specifically, not eating enough deeply colored fruits and vegetables, which are packed with essential vitamins and can help lower your cholesterol and blood pressure.
Solution: Spend big at the farmers’ market.
8. Lack of exercise. This one’s painfully obvious, like smoking, so don’t screw it up. Being young and healthy is no excuse for letting a week go by without raising your heart rate.
Solution: Cardiologists recommend at least 30 minutes of aerobic activity a day. See “Tune Up”(previous page) to make sure you’re getting the optimum amount.
9. Heredity. Sorry, this is the hand you’re dealt. Researchers recently identified a gene in people of European descent that increases the risk of heart disease 60 percent.
Solution: Until a genetic test is widely available, use this rule: If your father died of a heart attack before age 55 (or mother before 65), ask your doctor if you should get a stress test, which canreveal hidden coronary-artery disease.
Eat Like a Greek
One more reason to envy homeowners on Santorini: The incidence of coronary-artery disease in Mediterranean countries is among the world’s lowest. Researchers think diet is one of the reasons (lifestyle and social structure are others). A study published in the Annals of Internal Medicine concludes that Mediterranean diets lower risk factors such as blood pressure, fasting glucose levels, and C-reactive protein levels. More than 16 countries border the Med, and while there’s no one common diet among them, they do share a few staples:
(1) Virgin olive oil: Consume at least a tablespoon daily and your levels of good cholesterol will increase, meaning your risk for heart disease will decrease.
(2) Fish: Eat at least two servings of baked or grilled fish per week. The best kinds are high in omega-3 fatty acids, which have been shown to lower cholesterol; these include lake trout, salmon, mackerel, albacore tuna, and sardines.
(3) Fruits and vegetables: Residents of Greece average nine servings of fruits and vegetables per day.
(4) Red wine: Don’t get all Zorba about this; only a glass or two per day is recommended. Resveratrol, a powerful antioxidant, is more abundant in red wine than white.
(5) Nuts: Walnuts are particularly high in omega-3’s, but almonds, pecans, pistachios, and hazelnuts are also good sources.
(6) Whole grains: Mediterranean grains aren’t processed as much as those you find in the U.S., so they retain more nutrients. And skip the butter.
Live Well, Live Long
Heart Health Q & A
Do fish-oil supplements really prevent heart disease, or are they just a fad?The omega-3’s in fish oil help regulate cholesterol levels, which could decrease your risk of heart disease. “Fish oil lowers triglyceride levels,” says Dr. Brian Kahn, a cardiologist with Baltimore’s Mercy Medical Center. “We often recommend it in combination with statin drugs for patients with high cholesterol.” Kahn suggests taking 1,000 mg twice daily with your doctor’s approval. And check labels carefully: The best is distilled, pharmaceutical-grade fish oil that’s free of mercury and other toxins.
Live Well

You’ve eliminated the obvious risk factors, improved your diet, and maxed out your cardio training. Now what? The best thing you can do for your heart, we’re happy to report, is take a nap. Among other pleasant surprises.
Love Your Job
Get a better job, to be precise, and work less. According to a study published in the October 2006 issue of Hypertension┬Śone of our favorite reads┬Śclerical and unskilled workers are more likely to have high blood pressure than professionals, and the incidence of high blood pressure goes up with the number of hours worked each week. A separate study by researchers in Britain suggests that people who feel they are being treated unfairly┬Śat work or elsewhere┬Śalso have higher rates of heart disease.
Drink Up
Mounting evidence shows it’s better to drink in moderation than not at all. According to the Harvard School of Public Health and The New England Journal of Medicine, consuming one to two glasses of wine or beer a day reduces your chance of heart disease and stroke. (However, consuming more than three or four glasses a day is risky, they found.) Not a drinker? Try tea instead. Tea’s flavonoids have blood-thinning, artery-relaxing properties. But don’t add milk. A study published in January in the European Heart Journal found that milk negates tea’s beneficial effects, which may be one reason why tea drinkers in Asia have lower heart-disease rates than their counterparts in Britain.
Relax More
Go to your happy place. According to the Interheart global study, which surveyed 30,000 subjects across 52 countries, stress is responsible for a fifth of heart attacks worldwide. Duke University researchers found that among patients with a history of heart problems, stress management reduces cardiac events by 74 percent. Therapy, yoga, tai chi, and meditation are all effective techniques. Meditation especially “reduces excessive physiological responses to stressors,” notes Dr. Robert H. Schneider, co-author of Total Heart Health (Basic Health Publications, 2006).
Take a Nap
You snooze, you win. A study of more than 23,000 adults in Greece by the University of Athens and the Harvard School of Public Health found that subjects who regularly took midday siestas were 37 percent less likely to die of heart disease. That number increased to a whopping 64percent for working men who napped.
Eat Fat
No kidding. The American Heart Association recommends that 7 percent of your daily calories come from fat. Just make sure it’s the right kind. How do you know the good from the bad? Bad fats (saturated and trans fats) tend to be more solid at room temperature┬Śthink butter or animal fat┬Śwhile good fats (monounsaturated and polyunsaturated) tend to be moreliquid, as with olive and vegetable oils.
Floss Your Teeth
That’s right. The immediate gratification is nice, but it turns out there’s more to flossing. Studies published in the Journal of Periodontology show that people with periodontal disease are nearly twice as likely to suffer from coronary-artery disease. The theory is that oral bacteriacan enter the bloodstream and attach to fatty deposits in the heart’s blood vessels, leading to clots. The findings “support accumulating evidence that warding off oral bacteria may be good for your heart,” says Preston D. Miller Jr., DDS, president of the American Academy of Periodontology.